Understanding Type 1 Diabetes in Children
Monday, April 17, 2023
Eight-year old Braelynn Starnes is one of nearly 300,000 U.S. children living with type 1 diabetes. And unfortunately, misunderstandings, misconceptions, and even misdiagnoses are the reality for many children with type 1 diabetes.
“I want other people to know that I didn’t get type 1 diabetes from eating lots of sugar because kids in my class think that instead of me just being born with it,” she said. She was diagnosed with type 1 diabetes in 2021.
Confusion about this type of diabetes contributes to the unawareness of the crucial signs and symptoms. In certain illnesses, noticing the signs and symptoms can save lives, and type 1 diabetes is no different.
But by learning more about type 1 diabetes, you can help prevent misunderstanding and spread awareness of the warning signs.
Understanding Type 1 Diabetes in Children
Type 1 diabetes was once referred to as juvenile diabetes because it usually develops in children, teens, and young adults, but it can happen at any age. Type 1 diabetes occurs when the body produces little or no insulin. Insulin is a hormone responsible for regulating levels of glucose, or sugar, in the blood.
“Type 1 is technically the autoimmune form of diabetes. It is an 'oops' of the immune system,” said Amy Brant, wellness nurse and diabetes program manager at the Iredell Wellness & Diabetes Center.
Exposure to an environmental trigger, like a virus, illness, or traumatic event, may cause the immune system to turn on itself, destroying the body’s beta cells, the insulin-producing cells.
“Many times, we find that the child previously had some sort of virus or illness, like strep or the flu. Their body’s immune system was working really hard to fight off the virus, but instead of going after the virus, the bad guy, it goes after the beta cells of the pancreas,” said Brant.
According to the Centers for Disease Control and Prevention, this process of destroying the body’s beta cells can go on for months or years before any symptoms appear. But, once 90% of the beta cells are destroyed, symptoms can appear suddenly and can be severe.
Symptoms of type 1 diabetes typically include increased thirst, frequent urination, increased hunger, fatigue, and unexplained weight loss.
Braelyn’s Story
In Braelyn Starnes’ case, her mother noticed her symptoms very early, even before the typical signs were present.
“To be honest, COVID probably saved her. I am a teacher, and she was in kindergarten, and we both did online school that year, so we were really home together all the time. I started noticing she was ill after eating and complaining of headaches,” said Brittany Starnes, Braelyn’s mother.
When they went to Braelyn’s 7-year check-up in 2021, Brittany expressed her concerns to her pediatrician and asked if they could run a blood panel, a decision that would ultimately save Braelyn’s life. Around one week later, the pediatrician called and said Braelyn’s A1C level was elevated. An A1C test is a simple blood test that measures the average amount of sugar in the blood and is used to diagnose diabetes. She was referred to an endocrinologist but could not get an appointment until two months later.
However, at her appointment, the endocrinologist misdiagnosed Braelyn as a type 2 diabetic and recommended she change her diet.
Unfortunately, type 1 diabetes is often misdiagnosed. Signs can often be mistaken for type 2 diabetes, a urinary tract infection, or other common illnesses in children like the stomach bug or flu.
“Adults can articulate our symptoms. But with kids, when the doctor says, ‘how are you feeling’ and the child says, ‘I don't feel good,’ the doctor has to rely on the parent to give the symptoms, and sometimes if they don't say it just like the child is feeling, then it doesn’t flag right away. They just think it's a kids’ illness,” said Brant.
After changing her diet for six weeks, Brittany scheduled an appointment with another endocrinologist, who told them Braelyn did not, in fact, have type 2 diabetes. She had type 1.
“So we went through this whole 4-month stretch knowing her A1C was elevated and nothing being done about it, and then the next day, the world changed, and she was put on insulin,” said Brittany.
“She didn’t have the typical normal symptoms of type 1. Had it not been for COVID and us being at home together, she probably would have been the kid that ended up in the hospital, and that's when we would have found out. We caught it super early,” she added.
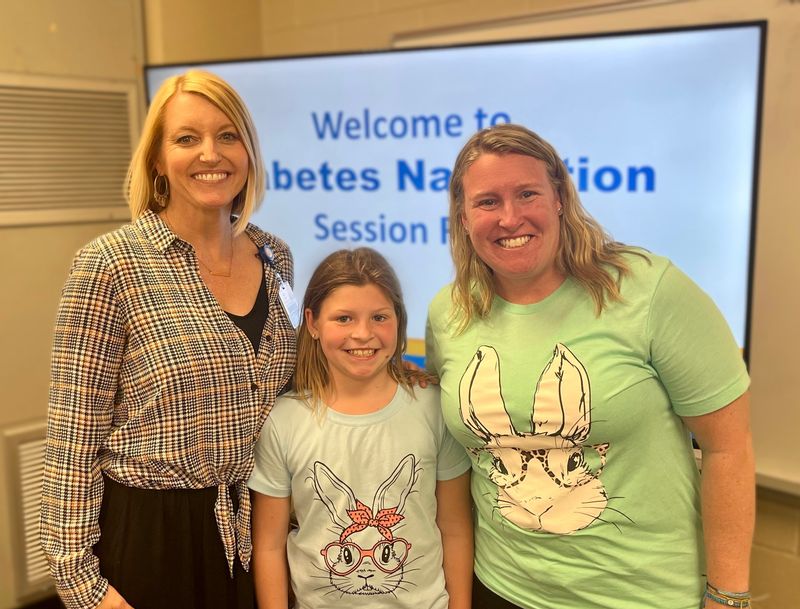
To learn more about her diagnosis and how to manage her diabetes properly, Braelyn and Brittany have been attending Iredell Health System’s Diabetes Navigation classes with Amy Brant.
Spreading Awareness
Brittany considers Braelyn blessed for never ending up in the hospital and catching it early. However, most children are hospitalized due to their symptoms. If your child does develop the telltale signs of type 1 diabetes—increased thirst, hunger, and urination—it’s important that you schedule a doctor’s appointment as soon as possible. If it is type 1 diabetes, the doctor’s office will likely send you to the hospital for IV fluids and insulin.
“The sooner you get to the hospital, the better. Definitely not any longer than 24 hours, but you’ll judge it based on how your child is doing,” said Brant.
When left undiagnosed, type 1 diabetes can develop into a life-threatening complication called diabetic ketoacidosis (DKA), the result of not enough insulin in the body. The signs of DKA include vomiting, nausea, shortness of breath, and a fruity smell on the breath. If untreated, DKA can lead to coma or death.
Since symptoms of type 1 diabetes do imitate many different illnesses, it’s crucial to request a blood sugar test just as Brittany did.
“Sometimes parents are quick to think their child is just sick. They’ll keep them home from school and let them rest for the day. But there are plenty of cases where it was left too long or was misdiagnosed in the emergency room with no blood sugar test, and it does result in death for some of these kids,” said Brant.
“Even if the doctor has no suspicion of diabetes whatsoever and there are other things that make more sense, always ask for that blood sugar check,” she added.
Learn More
To make an appointment with Amy Brant at the Iredell Wellness and Diabetes Center, please speak to your primary care provider about a referral. You can also call the diabetes center directly at 704-878-4556 and request they contact your provider.
Pictured: Amy Brant, Braelynn Starnes, Brittany Starnes.
Originally posted by Greater Statesville Chamber of Commerce via Locable
Greater Statesville Chamber of Commerce
116 N Center St
Statesville, NC 28677
704-873-2892
www.statesvillechamber.org

























